Crisis of Cancer Wait Times in the UK NHS
In 2023, England faced an unprecedented crisis in cancer waiting times, as revealed by a BBC News analysis. The report unveiled alarming statistics, with only 64.1% of patients commencing treatment within 62 days of suspected cancer diagnosis. This article examines the implications of prolonged cancer wait times within the UK's National Health Service (NHS), identifies contributing factors, and advocates for proactive measures to mitigate the crisis.
The Alarming Statistics
-
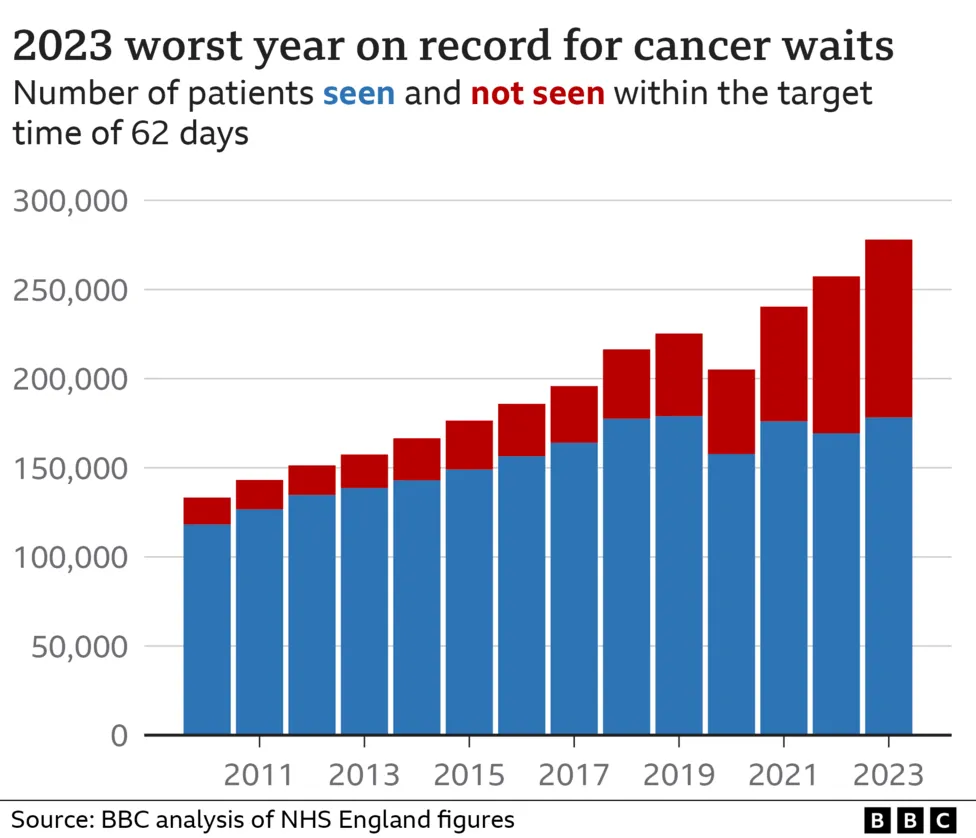
Cancer waiting times in 2023 reached their lowest point since records began, marking a continuous decline over the past 11 years.
-
Nearly 100,000 individuals experienced delays in life-saving cancer treatments, exacerbating anxieties and uncertainties during an already challenging period.
Understanding the Challenges
Several factors contribute to the crisis in cancer wait times:
-
The NHS faces capacity constraints exacerbated by rising cancer incidence rates and an aging population.
-
Insufficient resources, including staff and facilities, strain the healthcare system's ability to meet growing demand for cancer care.
Implications for Patient Care
Prolonged cancer wait times have profound implications for patient outcomes and well-being:
-
Patients endure prolonged periods of uncertainty, heightening emotional distress and anxiety.
-
Delayed access to treatment may compromise treatment efficacy and worsen prognoses for cancer patients.
Systemic Challenges
The crisis in cancer wait times reflects broader systemic challenges within the NHS:
-
Staff shortages across healthcare professions contribute to delays in cancer diagnosis and treatment initiation.
-
Operational inefficiencies and bureaucratic hurdles further impede timely access to cancer care services.
The Urgent Need for Reform
Addressing the crisis in cancer wait times demands comprehensive reform initiatives:
-
Increased funding and resource allocation are essential to expand capacity and enhance service provision.
-
Efforts to streamline referral pathways and improve care coordination can expedite cancer diagnosis and treatment initiation.
Stakeholder Responses
-
Organizations like Macmillan Cancer Support advocate for policy reforms to prioritise cancer care and support affected individuals.
-
NHS England acknowledges the challenges and emphasizes efforts to prioritise urgent cases amidst capacity strains.
Call to Action
The crisis in cancer wait times necessitates immediate action from policymakers, healthcare providers, and stakeholders:
-
Policymakers must prioritise cancer care within national health agendas and implement targeted interventions to improve wait times.
-
Stakeholders across the healthcare continuum must collaborate to address capacity constraints and streamline cancer care pathways.
Conclusion
The crisis in cancer wait times represents a critical juncture for the UK's NHS, underscoring the urgency of systemic reforms to ensure timely access to life-saving cancer care. By prioritising investment, fostering collaboration, and advocating for patient-centered approaches, stakeholders can work together to mitigate the crisis and uphold the NHS's commitment to equitable, quality healthcare for all.
Private Medical Insurance as a Potential Solution
Amidst the challenges facing the NHS, private medical insurance (PMI) emerges as a potential solution to alleviate strain on public healthcare services. PMI offers individuals the option to access timely medical care through private hospitals and clinics, bypassing lengthy wait times prevalent within the NHS.
Both for individuals and whole families, PMI provides peace of mind and expedited access to consultations, diagnostic tests, and treatments, including cancer care. While PMI may not address systemic issues within the NHS, it offers an alternative for individuals seeking prompt medical attention, complementing the public healthcare system and reducing pressure on NHS resources.